Signaling Molecules in Immune Responses and Inflammation Regulation
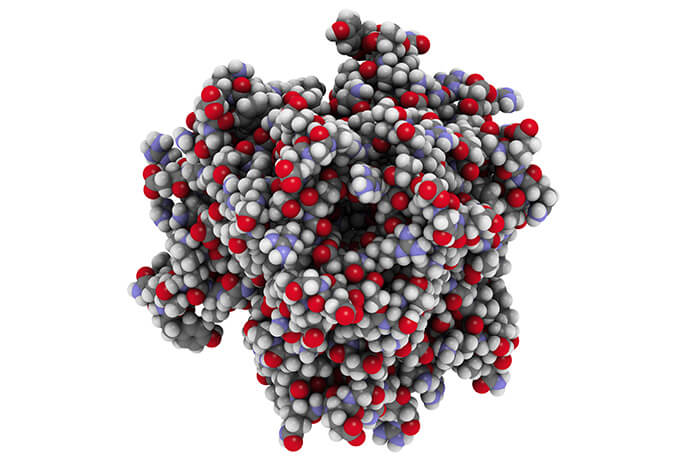
Cytokines stand as a fundamental class of signaling molecules that wield immense power in orchestrating the intricate symphony of the immune response and maintaining the delicate balance of inflammation within the human body. Functioning as molecular messengers, these small proteins transmit vital information among immune cells, tissues, and even organs, thereby exerting profound influences on immune regulation, inflammation, and overall health.
At their core, cytokines act as dynamic communicators within the immune system, conveying messages that dictate the initiation, coordination, and resolution of immune responses. Their signaling prowess extends across a spectrum of activities, ranging from cellular proliferation and differentiation to chemotaxis and immune cell activation. This intricate interplay shapes the immune system's ability to defend against pathogens, resolve infections, and promote tissue repair.
Crucially, cytokines possess the remarkable capacity to orchestrate inflammation—a double-edged sword that, when finely tuned, can be a lifesaving defense mechanism, but when dysregulated, can pave the way for chronic inflammatory diseases. In response to infections, injuries, or other immunological challenges, the immune system deploys an array of cytokines to summon immune cells to the scene of action, enhance their activity, and facilitate clearance of threats. However, when cytokine responses spiral out of control, chronic inflammation can ensue, contributing to conditions like autoimmune disorders and even tissue damage.
The regulation of cytokine production and activity is an artful balancing act that the immune system rigorously maintains. Homeostasis—the delicate equilibrium between proinflammatory and anti-inflammatory signals—is essential for optimal immune function and overall well-being. Any disruption to this equilibrium can lead to dire consequences, underscoring the critical importance of understanding cytokines' roles, functions, and dysregulation in various health contexts.
As we delve deeper into the world of cytokine analysis, we uncover not only the complexity of immune responses and inflammation but also the potential to harness this knowledge for therapeutic advancements. By scrutinizing the levels and interactions of these potent molecules, researchers and clinicians can gain unprecedented insights into disease pathways, treatment responses, and novel therapeutic targets.
Difference Between Proinflammatory and Inflammatory Cytokines
To comprehend the intricate landscape of cytokine signaling, it's crucial to distinguish between two pivotal categories: proinflammatory cytokines and inflammatory cytokines. While the terms might appear interchangeable at first glance, a closer inspection reveals their distinct roles in shaping immune responses and orchestrating the body's defense mechanisms.
Proinflammatory Cytokines: Igniting the Immune Response
Proinflammatory cytokines, as their name suggests, are the initiators and amplifiers of the immune response. These molecular messengers serve as the clarion call that rallies immune cells to the battlefield when the body encounters pathogens, injuries, or other threats. By delivering urgent messages to neighboring cells, proinflammatory cytokines instigate a cascade of events that collectively work to neutralize the challenge at hand.
Within the immune system's orchestra, proinflammatory cytokines act as the conductors, coordinating the activation of immune cells such as neutrophils, macrophages, and dendritic cells. They stimulate these cells to produce potent antimicrobial agents, engulf invaders, and present antigens to other immune cells. Furthermore, proinflammatory cytokines drive the expansion and differentiation of immune cells, amplifying the immune response's firepower.
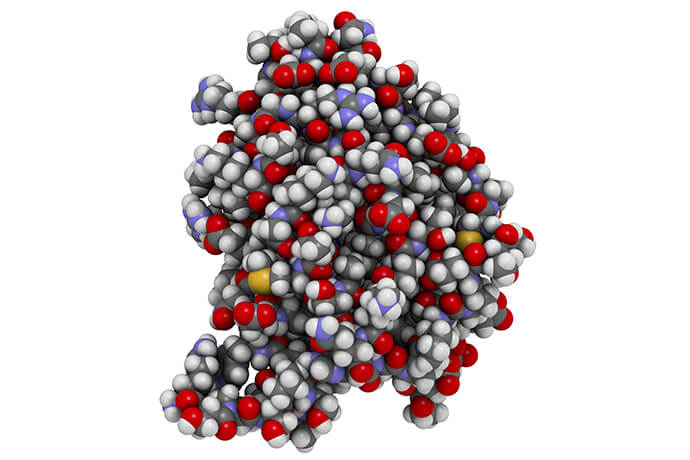
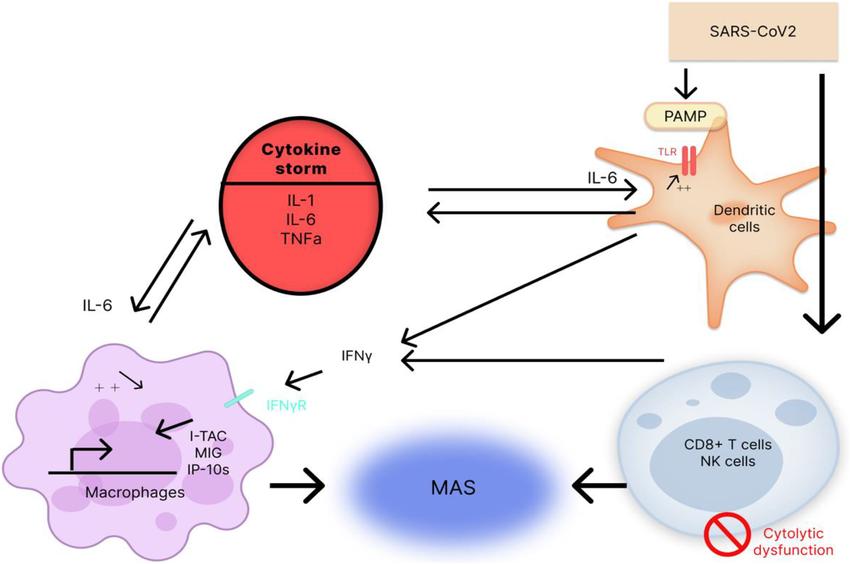 The influence of pro-inflammatory cytokines (IL-6, IL-1, and
TNFα) on the "cytokine storm" development and macrophage activation syndrome (MAS) under the effect of the
SARS-CoV-2 (Kirillova et al., 2022)
The influence of pro-inflammatory cytokines (IL-6, IL-1, and
TNFα) on the "cytokine storm" development and macrophage activation syndrome (MAS) under the effect of the
SARS-CoV-2 (Kirillova et al., 2022)
Inflammatory Cytokines: Balancing Act Between Repair and Regulation
Inflammatory cytokines, on the other hand, play a multifaceted role that extends beyond the initiation of immune responses. These cytokines participate in the delicate balance between promoting inflammation and orchestrating tissue repair. While inflammation might be associated with negative connotations due to its link to diseases, it's important to remember that controlled inflammation is an essential component of the healing process.
Inflammatory cytokines are instrumental in recruiting immune cells to the site of injury or infection, ensuring that damaged tissues receive the necessary attention. Additionally, they stimulate fibroblasts to synthesize collagen, a crucial protein for tissue healing. In this way, inflammatory cytokines guide the reparative efforts of the immune system, aiding in wound closure and tissue regeneration.
However, the key to harnessing the beneficial aspects of inflammation lies in the balance between proinflammatory and anti-inflammatory signals. Dysregulation of this equilibrium can lead to chronic inflammation, tissue damage, and autoimmune disorders. Inflammatory cytokines are central to maintaining this equilibrium by modulating the intensity and duration of immune responses, thus preventing excessive tissue destruction.
Select Services
Key Proinflammatory Cytokines
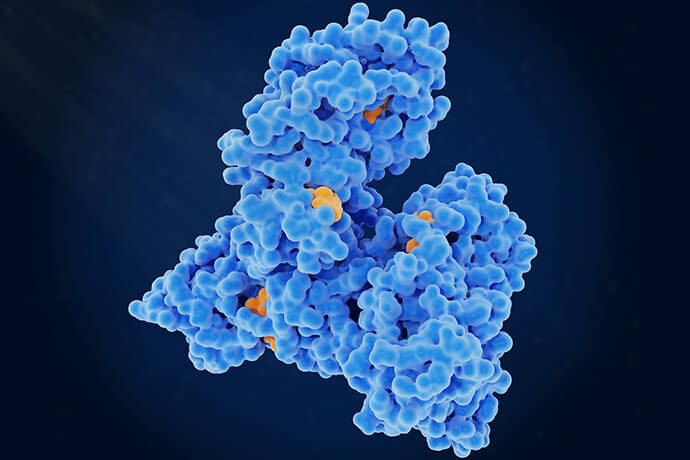
Proinflammatory cytokines form a crucial armamentarium in the immune system's arsenal, swiftly responding to threats and orchestrating the body's defense against infections and injuries. Let's explore some of the prominent players in this category: Interleukin-1 (IL-1), Interleukin-6 (IL-6), Tumor Necrosis Factor-alpha (TNF-α), and Interleukin-12 (IL-12).
| Proinflammatory Cytokine | Role | Sources | Effects on Immune Cells |
|---|---|---|---|
| Interleukin-1 (IL-1) | Initiates inflammatory cascade, activates immune cells, promotes fever | Monocytes, macrophages, dendritic cells, various immune and non-immune cells | Enhances neutrophil recruitment, immune cell activation, and fever induction |
| Interleukin-6 (IL-6) | Modulates immune cell activation, supports acute phase response, influences B cell maturation | Macrophages, T cells, fibroblasts, various cells | Stimulates acute phase protein production, enhances antibody production, regulates inflammation |
| Tumor Necrosis Factor-alpha (TNF-α) | Triggers immune cell activation, vessel permeability, apoptosis | Macrophages, immune cells | Activates immune cells, promotes cytokine release, regulates cell death |
| Interleukin-12 (IL-12) | Orchestrates immune responses against intracellular pathogens, drives Th1 differentiation | Dendritic cells, macrophages | Stimulates IFN-γ production, enhances cellular immunity |
Prominent Inflammatory Cytokines
Inflammatory cytokines constitute a diverse group of signaling molecules that exert significant influence on immune responses, tissue repair, and overall inflammatory processes. Among the notable players in this category are Interleukin-8 (IL-8), Interleukin-17 (IL-17), and Interleukin-23 (IL-23).
| Inflammatory Cytokine | Role | Contribution to Inflammation | Effect on Tissue Damage |
|---|---|---|---|
| Interleukin-8 (IL-8) | Chemokine guiding neutrophil recruitment | Essential for immune defense by attracting neutrophils | Excessive IL-8 can lead to tissue damage due to neutrophil-generated enzymes |
| Interleukin-17 (IL-17) | Promotes immune cell recruitment and activation | Amplifies immune response by inducing cytokine and chemokine production | Persistent IL-17 elevation can cause chronic inflammation and tissue damage |
| Interleukin-23 (IL-23) | Drives Th17 differentiation and expansion | Supports immune response via Th17 cells producing proinflammatory cytokines | Dysregulation may lead to excessive inflammation and tissue destruction |
Regulation and Dysregulation of Proinflammatory and Inflammatory Cytokines
Balanced Regulation: The Key to Immune Harmony
Proinflammatory Cytokines: In controlled amounts, proinflammatory cytokines initiate and amplify immune responses against threats. They rally immune cells, stimulate inflammation, and direct the immune system's focus toward targets.
Inflammatory Cytokines: Inflammatory cytokines contribute to inflammation and immune cell recruitment, aiding tissue repair and clearance of infections. They maintain a delicate balance between promoting inflammation and fostering healing.
Dysregulation and its Consequences: Immune Dysfunctions Unleashed
Proinflammatory Cytokines:
When the regulation of proinflammatory cytokines is disrupted, the immune response can spiral out of control, leading to chronic inflammation. Excessive production of proinflammatory cytokines can result in a constant state of immune activation, causing damage to healthy tissues over time. Chronic inflammatory diseases like rheumatoid arthritis, psoriasis, and inflammatory bowel diseases can arise as a consequence.
Inflammatory Cytokines:
Dysregulation of inflammatory cytokines, like IL-8, IL-17, and IL-23, can disturb the balance between immune response and tissue repair. Prolonged elevation of these cytokines can lead to the recruitment of immune cells that cause collateral damage to tissues, contributing to the development of autoimmune diseases such as multiple sclerosis and systemic lupus erythematosus.
Autoimmune Diseases: The Dysregulation Connection
Proinflammatory Cytokines:
Dysregulation of proinflammatory cytokines can lead to the breakdown of immune tolerance. When the immune system loses its ability to distinguish between self and non-self, it can mistakenly attack the body's own tissues. This phenomenon underlies autoimmune diseases like rheumatoid arthritis, where TNF-α's dysregulation contributes to joint inflammation and damage.
Inflammatory Cytokines:
Elevated levels of inflammatory cytokines, particularly IL-17, can exacerbate autoimmune responses. The chronic presence of IL-17-driven inflammation is associated with tissue damage in autoimmune conditions such as psoriasis, where skin lesions develop due to immune cell infiltration.
Cytokine Analysis Techniques: Unveiling the Tools for Precision Measurement
The remarkable complexity of cytokine signaling demands sophisticated techniques for accurate measurement. Researchers and clinicians rely on a range of methods to dissect cytokine profiles and gain insights into immune responses. One prominent approach is the use of Luminex multiplex assays, among other techniques. Luminex multiplex assays revolutionized cytokine analysis by enabling the simultaneous measurement of multiple cytokines from a single sample. This technology employs microspheres coated with unique fluorescent dyes, each designed to capture a specific cytokine. By tagging different cytokines with distinct dyes, researchers can measure multiple cytokines in a single assay, saving time and resources.
Advantages of Luminex Multiplex Assays
High Throughput: Luminex technology can measure dozens of cytokines simultaneously in a single sample, accelerating data acquisition.
Small Sample Size: These assays require only small amounts of biological material, conserving precious samples.
Precision and Sensitivity: Luminex assays offer high sensitivity, enabling the detection of cytokines even at low concentrations.
Data-rich Insights: Researchers obtain comprehensive cytokine profiles, facilitating a more holistic understanding of immune responses.
Reference:
- Kirillova, Aleksandra, Anna Lado, and Nataliya Blatt. "Application of Monoclonal Antibody Drugs in Treatment of COVID-19: A Review." Bionanoscience 12.4 (2022): 1436-1454.