What is C-reactive protein (CRP)?
Definition and Structure of CRP
C-reactive protein (CRP) is a key acute-phase reactant and a major biomarker of inflammation in humans. It belongs to the pentraxin family of proteins, characterized by its pentameric structure composed of five identical subunits. Each subunit consists of 206 amino acids and includes a calcium ion that stabilizes its disc-shaped configuration. CRP exists in two forms: native CRP (nCRP) and modified CRP (mCRP). While nCRP circulates in a pentameric state, mCRP undergoes conformational changes upon binding to specific ligands, enhancing its biological activity in the immune response.
Production and Release Mechanisms
The production of CRP is primarily regulated by hepatocytes in response to cytokines, particularly interleukin-6 (IL-6), during acute-phase responses. Upon encountering inflammatory stimuli, such as tissue injury or infection, immune cells release IL-6 into the bloodstream. IL-6 binds to specific receptors on hepatocytes, activating signaling pathways that lead to the transcription and translation of CRP mRNA. This results in the rapid synthesis and secretion of CRP into the bloodstream within hours of the initial stimulus. CRP levels peak between 36 to 50 hours post-stimulation and decline as inflammation resolves. Clearance of CRP from circulation occurs through receptor-mediated endocytosis by hepatocytes and macrophages, contributing to the regulation of its serum levels.
Understanding the structural composition and dynamic regulation of CRP production provides insights into its role as a sensitive marker of inflammation and tissue damage in clinical settings. Laboratory techniques, such as enzyme-linked immunosorbent assay (ELISA) and immunoturbidimetry, enable accurate measurement of CRP levels, facilitating its diagnostic utility across various inflammatory conditions.
Role in the Body's Immune Response and Inflammation
Opsonization and Phagocytosis: One of CRP's primary functions is to recognize and bind to phosphocholine residues exposed on the surface of damaged cells, apoptotic cells, and microbial pathogens. This binding facilitates the activation of the complement system via the classical pathway. CRP binds to C1q, the first component of the complement cascade, leading to the formation of C1q-CRP complexes. These complexes trigger a series of enzymatic reactions that result in the deposition of complement components C3b and C4b on the target surface. These components, in turn, promote opsonization, enhancing the recognition and phagocytosis of pathogens by macrophages and neutrophils. This process plays a crucial role in the clearance of cellular debris and infectious agents, thereby promoting tissue repair and resolution of inflammation.
Modulation of Inflammatory Responses: In addition to its role in complement activation, CRP interacts with various cellular receptors, including Fcγ receptors on phagocytic cells and receptors on endothelial cells. By binding to these receptors, CRP modulates inflammatory signaling pathways, leading to the production of cytokines, chemokines, and adhesion molecules. This enhances leukocyte recruitment to sites of inflammation and promotes the local inflammatory response. Furthermore, CRP can directly stimulate the release of cytokines such as interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α), and interleukin-6 (IL-6) from monocytes and macrophages, amplifying the inflammatory cascade.
Regulation of Endothelial Function: CRP also influences endothelial cell function by promoting the expression of adhesion molecules (e.g., ICAM-1, VCAM-1) and tissue factor, which are involved in leukocyte adhesion and thrombosis. This endothelial activation contributes to the pathogenesis of vascular diseases such as atherosclerosis and thrombosis, where CRP levels are elevated.
Select Service
Clinical Significance and Conditions Associated with Elevated CRP Levels
C-reactive protein (CRP) serves as a critical biomarker in clinical practice, reflecting systemic inflammation and tissue damage across a spectrum of acute and chronic conditions. Elevated CRP levels are indicative of underlying pathophysiological processes and play a significant role in disease diagnosis, prognosis, and therapeutic monitoring.
Infectious Diseases: CRP is a sensitive marker of acute bacterial, viral, fungal, and parasitic infections. During infection, immune cells release pro-inflammatory cytokines, notably interleukin-6 (IL-6), which stimulates hepatocytes to produce CRP. Elevated CRP levels in these scenarios reflect the intensity of the host immune response and aid clinicians in differentiating between infectious and non-infectious causes of fever or systemic symptoms.
Autoimmune Disorders: Chronic autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus (SLE), and inflammatory bowel diseases (IBD), are characterized by persistent inflammation and immune dysregulation. Elevated CRP levels in these conditions correlate with disease activity and severity. Monitoring CRP helps assess response to immunosuppressive therapies and guide treatment decisions in autoimmune disorders.
Cardiovascular Diseases: CRP is associated with the pathogenesis of cardiovascular diseases, including atherosclerosis, myocardial infarction, and stroke. Inflammatory processes contribute to the development and progression of vascular endothelial dysfunction and plaque formation. Elevated CRP levels serve as a prognostic marker for cardiovascular events and can aid in risk stratification among individuals with coronary artery disease and other cardiovascular risk factors.
Chronic Inflammatory Conditions: Various chronic inflammatory conditions, such as chronic obstructive pulmonary disease (COPD), inflammatory bowel diseases (IBD), and chronic kidney disease, exhibit sustained elevation of CRP levels. Monitoring CRP helps clinicians assess disease progression, evaluate treatment efficacy, and predict outcomes in these chronic inflammatory states.
Cancer: Certain malignancies, particularly those associated with chronic inflammation or tissue necrosis, can lead to elevated CRP levels. CRP serves as a marker of cancer-related inflammation and is associated with tumor progression, metastasis, and poor prognosis in some cancer types. Monitoring CRP levels may provide insights into disease activity and response to cancer therapies.
Other Conditions: Elevated CRP levels have been observed in metabolic disorders (e.g., obesity, metabolic syndrome), neurological diseases (e.g., Alzheimer's disease), and severe trauma or burns. In these contexts, CRP serves as a non-specific marker of systemic inflammation and tissue injury, contributing to the overall assessment of disease severity and patient management.
What is PCT?
Procalcitonin (PCT) is a peptide precursor of the hormone calcitonin, primarily synthesized in extra-thyroidal tissues in response to bacterial infections and inflammatory stimuli. Unlike calcitonin, which regulates calcium homeostasis, PCT is not biologically active under normal conditions but serves as a valuable biomarker in clinical practice due to its specific response to bacterial infections.
Structure and Synthesis of PCT
Procalcitonin is encoded by the CALC-1 gene and synthesized predominantly in the liver and, to a lesser extent, in peripheral tissues such as lung, kidney, and intestine. It is synthesized as a 116-amino acid precursor peptide, which undergoes post-translational modifications to form the mature PCT molecule. During bacterial infections, inflammatory cytokines, particularly interleukin-6 (IL-6), interleukin-1 beta (IL-1β), and tumor necrosis factor-alpha (TNF-α), stimulate PCT production and release into the bloodstream.
Role as a Biomarker for Bacterial Infections
PCT levels rise rapidly and significantly in response to bacterial infections, making it a valuable biomarker for distinguishing bacterial infections from non-infectious causes of inflammation, such as viral infections or autoimmune disorders. Unlike C-reactive protein (CRP), which is a non-specific marker of inflammation, PCT exhibits higher specificity for bacterial infections. The magnitude of PCT elevation correlates with the severity and extent of bacterial involvement, aiding clinicians in the early diagnosis, risk stratification, and monitoring of bacterial sepsis and other systemic infections.
Regulation and Clearance of PCT
In healthy individuals, basal levels of PCT are low (<0.1 ng/mL) but can increase rapidly during bacterial infections, with peak concentrations reached within 6 to 24 hours after the onset of infection. PCT levels decline rapidly upon initiation of effective antibiotic therapy or resolution of the bacterial infection, reflecting its short half-life of approximately 24 hours. Hepatocytes and renal clearance mechanisms contribute to the rapid elimination of PCT from circulation once the inflammatory stimulus diminishes.
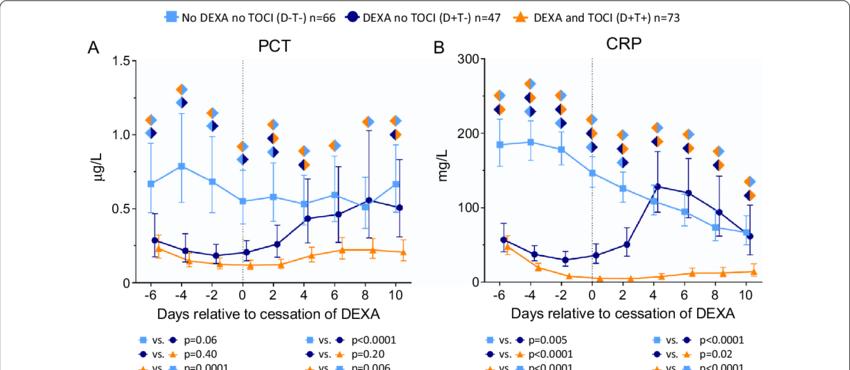 Levels of a procalcitonin (PCT) and b C-reactive protein (CRP) over time within 6 days prior to and 10 days following cessation of dexamethasone (DEXA) in the group of patients treated with neither dexamethasone nor tocilizumab (D−T− group) as well as in the D+T− and D+T+ groups (Kooistra et al., 2021).
Levels of a procalcitonin (PCT) and b C-reactive protein (CRP) over time within 6 days prior to and 10 days following cessation of dexamethasone (DEXA) in the group of patients treated with neither dexamethasone nor tocilizumab (D−T− group) as well as in the D+T− and D+T+ groups (Kooistra et al., 2021).
Comparison of CRP and PCT
| Feature | CRP (C-reactive protein) | PCT (procalcitonin) |
|---|---|---|
| Definition | CRP is an acute-phase protein produced by the liver in response to inflammation. | PCT is the precursor peptide of calcitonin, primarily produced by several tissues during bacterial infections. |
| Role in the Body | Indicator of inflammation and tissue damage. | Marker for bacterial infections, especially sepsis. |
| Production Site | Liver hepatocytes | Various tissues (e.g., liver, lung) during bacterial infections. |
| Production Mechanism | Synthesized in the liver mainly in response to IL-6 release. | Synthesized in several tissues (e.g., liver, lung) under the influence of bacterial endotoxins and cytokines. |
| Release Mechanism | Released rapidly in response to inflammatory stimuli. | Levels increase significantly in bacterial infections. |
| Half-life | ~19 hours | ~24 hours (shorter in patients with severe sepsis/septic shock) |
| Diagnostic Utility | Widely used as a general marker of inflammation. | Specific marker for bacterial infections, aiding in diagnosis and monitoring treatment. |
| Clinical Applications | Assessing disease activity in conditions like rheumatoid arthritis, cardiovascular disease. | Diagnosing and monitoring bacterial infections, guiding antibiotic therapy. |
| Dynamic Range | Broad range, reflecting systemic inflammation | Narrower range, directly correlating with bacterial load |
| Clinical Cut-off Values | Varies by assay and condition (e.g., >10 mg/L for general inflammation). | Elevated levels (>0.5 ng/mL) indicate bacterial infection. |
| Advantages | Broad applicability in assessing inflammatory conditions. | Highly specific for bacterial infections, aiding in targeted therapy. |
| Limitations | Non-specific elevation in various conditions (e.g., trauma). | Levels may be influenced by non-infectious conditions like surgery and trauma. |
| Research and Development | Ongoing studies into its role in predicting cardiovascular risk. | Continued research into its utility in differentiating bacterial infections from other causes of inflammation. |
Methods for CRP and PCT Measurement
CRP Measurement Methods
- Enzyme-Linked Immunosorbent Assay (ELISA): ELISA employs specific antibodies to detect and quantify CRP levels in serum or plasma. This method provides robust sensitivity and is widely used in clinical laboratories for its reliability in measuring a broad range of CRP concentrations.
- Immunoturbidimetry and Nephelometry: These automated methods measure the turbidity or light scattering caused by antigen-antibody complexes formed between CRP and specific antibodies. They offer rapid results and are suitable for high-throughput settings, ensuring precise quantification of CRP levels.
- Luminex xMAP Technology: Luminex xMAP utilizes fluorescently coded microspheres to simultaneously measure multiple analytes, including CRP, in a single sample. This multiplexing capability enhances throughput and efficiency, allowing for the simultaneous analysis of various biomarkers with high sensitivity and specificity.
PCT Measurement Methods
- Enzyme-Linked Fluorescence Assay (ELFA): ELFA combines ELISA principles with fluorescence detection to measure PCT levels. It provides rapid results and high sensitivity, making it ideal for critical care settings where timely diagnosis is crucial.
- Chemiluminescent Immunoassay (CLIA): CLIA detects PCT based on chemiluminescent reactions between labeled antibodies and PCT molecules. This method offers excellent sensitivity and a broad dynamic range, ensuring accurate measurement of PCT in clinical samples.
- Luminex xMAP Technology: Similar to its application in CRP measurement, Luminex xMAP is utilized for multiplex analysis of PCT and other biomarkers. It enables simultaneous detection and quantification of multiple analytes in a single sample, providing comprehensive insights into inflammatory and infectious conditions.
Select Service
Applications of CRP and PCT Assays in Clinical Practice
CRP (C-reactive Protein) Assay
General Inflammation Monitoring:
CRP levels are routinely measured to assess and monitor inflammatory conditions such as rheumatoid arthritis, inflammatory bowel disease, and autoimmune disorders. Elevated CRP indicates ongoing inflammation and disease activity.
Cardiovascular Risk Assessment:
CRP serves as a biomarker for cardiovascular diseases (CVD), reflecting systemic inflammation linked to atherosclerosis and heart disease. High CRP levels are associated with increased CVD risk, guiding risk stratification and preventive measures.
Infectious Diseases:
In infectious diseases, CRP levels help monitor disease progression and response to treatment. While less specific than PCT for bacterial infections, elevated CRP can indicate severe infections or complications requiring intensive care.
PCT (Procalcitonin) Assay
Bacterial Infections:
PCT is highly specific for bacterial infections and aids in distinguishing bacterial from viral infections. Rapid elevation of PCT levels within hours of infection onset supports early diagnosis and timely initiation of antibiotic therapy.
Sepsis Management:
In critically ill patients, PCT levels correlate with the severity of sepsis and guide antibiotic treatment duration. Serial PCT measurements help monitor treatment response and identify complications such as septic shock.
Lower Respiratory Tract Infections:
PCT is particularly valuable in diagnosing and managing lower respiratory tract infections, such as pneumonia. It helps clinicians decide on antibiotic therapy, reducing unnecessary antibiotic use and associated risks.
Reference:
- Kooistra, Emma J., et al. "Dexamethasone and tocilizumab treatment considerably reduces the value of C-reactive protein and procalcitonin to detect secondary bacterial infections in COVID-19 patients." Critical Care 25 (2021): 1-12.